Most people wait until something feels wrong before checking their health. But here’s the truth: by the time symptoms show up, your body has often been out of balance for months or even years. That’s where annual blood work and key health markers come in.
They act like a report card for your health, helping you catch small problems before they become major ones.
Metabolic Health Crisis In America:
Here’s a startling reality: 93% of Americans are not metabolically healthy.
Using data from the National Health and Nutrition Examination Survey (NHANES, 1999–2018), researchers found that only 1 in 14 U.S. adults had optimal levels of all five metabolic risk factors:
Body Mass Index (BMI)
Blood glucose
Blood pressure
HDL cholesterol
Triglycerides
Only 37% of adults had fasting glucose under 100 mg/dL, the typical threshold for prediabetes. That means the majority of Americans are walking around with silent metabolic dysfunction, often with no obvious symptoms.
As a registered dietitian with nearly two decades of experience, what I wish every patient knew about their blood work is simple: don’t wait until there’s a problem. Taking a proactive approach means tracking your health markers regularly, watching trends over time, and making changes before medications are prescribed or serious conditions develop.
At Healthy Steps Nutrition, we believe health is the outcome of habits. When you focus on a holistic approach — nutrition, exercise, sleep, stress management, and support systems — you’re not just improving your lifestyle, you’re improving the very markers that predict long-term health.
That’s why understanding your body composition and blood markers is so important. These numbers provide a clear window into how your body is functioning today and where it may be headed tomorrow. In this blog, we’ll break down what these markers mean, why they matter, and the practical steps you can take to improve them, starting with body composition.
Body Composition:
While weight and BMI are commonly used, body fat percentage gives a much clearer picture of health. It distinguishes between fat mass, muscle mass, and water weight and tells us whether your weight is being carried in a healthy or risky way.
Body Fat Percentage

Why Women’s Recommended Body Fat Is Higher Than Men’s:
Essential fat: Women naturally need 10–12% essential fat (compared to men’s 2–4%) to support reproductive function, hormone regulation, and overall health.
Hormones: Estrogen and progesterone play key roles in fat storage, especially around the hips and thighs, which is protective.
Visceral fat: Both men and women are at risk when fat accumulates around the organs (visceral fat), but men tend to carry more fat in the abdominal area, which increases heart disease and diabetes risk
Risks of High Body Fat (especially visceral fat):
Metabolic syndrome (high waist circumference, high triglycerides, low HDL, high blood pressure, high glucose)
Type 2 diabetes
Cardiovascular disease (heart attack, stroke)
Non-alcoholic fatty liver disease (NAFLD)
Certain cancers (breast, colon)
Tips When Testing Body Fat:
Retest every month to track progress
Do it first thing in the morning, before exercise, and while hydrated for the most accurate results
Dehydration skews results: muscle mass will appear lower, and body fat will appear higher
Body Mass Index: BMI
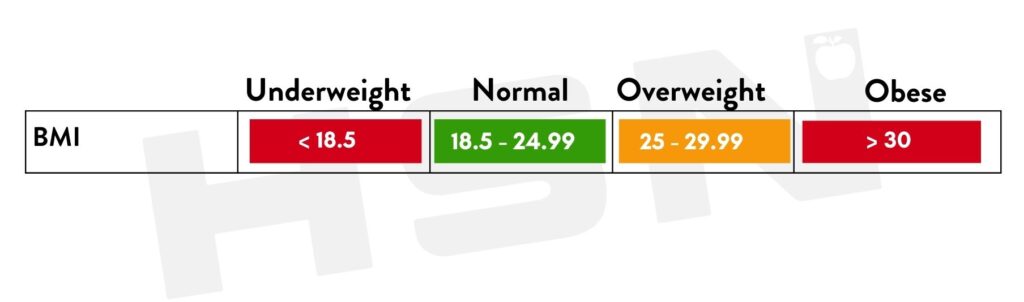
Body Mass Index (BMI) is one of the most common health measures used in medical settings. It’s calculated by dividing your weight (kg) by height (m²) and categorizes you as underweight, normal weight, overweight, or obese.
Why BMI Falls Short:
Doesn’t measure body fat directly: An athlete with high muscle mass may fall into the “overweight” or “obese” category despite being metabolically healthy.
Doesn’t account for fat distribution: Visceral fat (around organs) is far riskier than subcutaneous fat (under the skin), but BMI cannot distinguish between the two.
Doesn’t reflect body composition changes: Losing fat and gaining muscle may not shift BMI much, but it dramatically improves health.
BMI can be a starting point, but it should never be the end point. Pairing BMI with body composition testing (body fat %, muscle mass, water weight) and blood markers provides a far more accurate picture of your overall health.
What Are Health Markers?
Health markers are measurable numbers from your body, such as blood sugar, cholesterol, or body fat, that reflect your current state of health. They help identify:
Metabolic health (blood sugar, triglycerides, cholesterol)
Organ function (liver, kidneys)
Nutrient levels (vitamin D, iron)
Hormonal balance
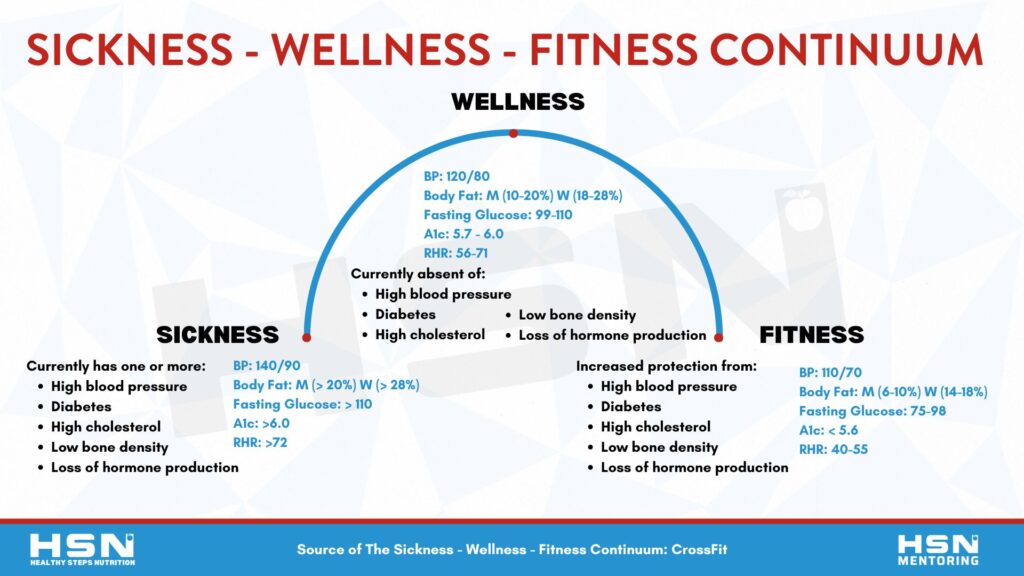
When tracked over time, these numbers highlight trends that show whether you’re moving toward sickness, staying in wellness, or thriving in fitness.
What To Know Before Getting Your Bloodwork Done:
How Often Should You Get Your Bloodwork Done?
At a minimum: Once per year (annual check-up)
Every 6–9 months: If you’re making lifestyle changes or have a family history of chronic disease
Every 3–4 months: If managing diabetes, thyroid, or other chronic conditions
Best Practices Before Testing
Fast 8–12 hours (water only)
Be hydrated
Get a good night’s sleep (7–9 hours)
Schedule testing in the morning for consistency
Health Markers To Watch
Understanding your blood work numbers is one of the most powerful steps you can take toward better health. These markers act like your body’s dashboard, showing how well your metabolism, heart, and overall health are functioning. While one number alone doesn’t tell the full story, looking at them together can highlight risks early and guide smarter lifestyle choices. Below is a quick reference chart to help you see the difference between healthy, borderline, and unhealthy ranges for some of the most important markers you should know.

Fasting Glucose
What Is It?
Measures the amount of sugar (glucose) in your blood after you haven’t eaten for at least 8 hours.
Used to assess:
- Blood sugar regulation
- Insulin sensitivity
- Risk of prediabetes, diabetes, and metabolic dysfunction
What Causes It To Be Elevated?
- Poor sleep
- High stress (raises cortisol → increases glucose)
- Eating late at night or large meals before bed
- Low physical activity
- Dehydration
- Insulin resistance or prediabetes
- Chronic inflammation
What Causes It To Be Low?
- Prolonged fasting or skipping meals
- Overuse of insulin or diabetes meds
- High insulin sensitivity
- Hormonal dysregulation (e.g., adrenal fatigue, reactive hypoglycemia)
- Intense exercise without enough recovery/fuel
A1c: 3-Month Average Of Your Blood Sugar
What Is It?
Measures your average blood sugar levels over the past 2 to 3 months. It does this by measuring the percentage of red blood cells that have sugar (glucose) “stuck” to them.
Since red blood cells live about 90–120 days, A1C gives you a long-term view of blood sugar control, unlike fasting glucose, which is just a snapshot.
What It Matters?
- Reflects long-term blood sugar control
- Used to diagnose or monitor prediabetes and type 2 diabetes
- High A1C = higher risk for: Heart disease, stroke, kidney damage, nerve damage, and vision loss
- Even in the “normal” range, higher A1C may predict metabolic dysfunction
What Causes It To Be High?
- A diet high in sugar and refined carbs
- Infrequent or low activity levels
- Insulin resistance
- Chronic stress (via cortisol)
- Poor sleep
- Certain medications or conditions (PCOS, liver disease)
Tips To Improve Fasting Glucose and A1c:
Balanced meals, pairing protein with every meal
The plate method
Limit sugar and ultra-processed foods
Walking after meals
Sleep: 7-9 hours per night
Strength training
Take Control Of Your Blood Sugar
With Continuous Glucose Monitoring
Elevated blood sugar is the root cause of many chronic diseases, from type 2 diabetes to heart disease and fatty liver. At Healthy Steps Nutrition, we offer a Blood Sugar Balance Specialty program with Continuous Glucose Monitoring (CGM) designed to help you take control of your health before it’s too late.
What’s Included in the Program:
12 weeks of Personalized nutrition coaching with a registered dietitian
Four weeks of continuous glucose monitoring (real-time data on how your body responds to food, stress, and exercise)
Weekly Zoom sessions to review results, tweak your nutrition plan, and directly improve blood sugar management
Who Is This Program For?
- Individuals with a family history of diabetes
- People with borderline blood sugar but not yet diagnosed with diabetes
- Anyone looking to gain a deeper understanding of how their body works and how to take control of their health
If you’ve been wondering how your lifestyle choices impact your blood sugar and long-term health, this program gives you the answers and the tools to improve.
Triglycerides
What Is It?
Triglycerides are a type of fat (lipid) in your blood.
After you eat, your body converts extra calories, especially from carbs and sugar, into triglycerides and stores them in fat cells. Later, hormones release them for energy between meals.
What Causes It To Be High?
- Excess sugar & refined carbs (soda, desserts, white bread)
- Too much alcohol
- Overeating calories in general
- Sedentary lifestyle
- Uncontrolled diabetes or insulin resistance
- Certain meds (beta-blockers, steroids, diuretics)
- Genetics (familial hypertriglyceridemia)
What Causes It To Be Low?
- Very low-fat diet
- Malnutrition or malabsorption
- Overactive thyroid (hyperthyroidism)
Tips To Improve Triglycerides:
Balanced meals, pairing protein with every meal
Limit alcohol and don’t smoke
Prioritize fiber
Walking after meals
Increase omega-3 intake
Strength training
HDL
What Is It?
HDL stands for High-Density Lipoprotein.
Think of HDL as your body’s cholesterol cleanup crew: it carries cholesterol away from your arteries and back to your liver, where it can be processed and removed.
That’s why higher HDL levels are protective against heart disease.
Why It Matters?
- HDL is protective because it clears cholesterol from the arteries
- Low HDL + high triglycerides = strong predictor of metabolic syndrome and cardiovascular risk
- Raising HDL through healthy lifestyle changes is one of the best ways to protect long-term heart health
What Causes It To Be Low? (Not A Good Thing)
- High intake of refined carbs and sugar
- Sedentary lifestyle
- Smoking
- Excess alcohol
- Being overweight or insulin-resistant
- Genetic factors
Tips To Improve HDL Levels:
Limit alcohol and don’t smoke
Balanced diet with primarily whole foods
30+ grams of fiber per day
Walking after meals
Increase omega-3 intake
Strength training
LDL
What Is It?
It carries cholesterol particles through your bloodstream. When LDL levels are too high, cholesterol can build up in artery walls → forming plaques that increase the risk of heart attack and stroke.
Not all LDL is the same:
- Small, dense LDL = more harmful (more likely to penetrate artery walls).
- Large, fluffy LDL = less dangerous.
Unfortunately, a standard lipid panel only shows total LDL, not particle size.
Why It Matters?
- High LDL is a major risk factor for atherosclerosis, heart attack, and stroke
- But context matters: HDL, triglycerides, inflammation (CRP), and lifestyle paint the full picture
What Causes It To Be High?
- Diets high in saturated fats (fatty cuts of meat, butter, cheese)
- Trans fats (processed & fried foods)
- High sugar and refined carbs (can increase small, dense LDL)
- Genetics (familial hypercholesterolemia)
- Lack of physical activity
- Smoking
- Obesity and insulin resistance
Tips To Lower LDL Levels:
30+ grams of fiber per day
Limit sugar and ultra-processed food
Limited fried foods
Exercising regularly
Maintain a healthy weight
Sleep 7-8 hours per night
Manage stress
Vitamin D
What Is It?
Vitamin D is actually a hormone-like vitamin that plays a vital role in:
- Bone health (helps absorb calcium & phosphorus)
- Immune system function
- Muscle strength & recovery
- Mood regulation (linked to depression risk)
- Inflammation control
Why It Matters?
- Low vitamin D is linked to weaker bones, poor immunity, increased risk of infections, mood disorders, and even metabolic issues.
- It’s one of the easiest nutrients to optimize with sunlight, food, and supplementation.
What Causes It To Be Low?
- Lack of sun exposure (the most common cause)
- Living in northern latitudes or using lots of sunscreen
- Darker skin (higher melanin reduces vitamin D synthesis)
- Diets low in vitamin D (few foods naturally contain it)
- Obesity (vitamin D is fat-soluble and gets trapped in fat tissue)
- Malabsorption issues (celiac, Crohn’s, gastric bypass)
Tips To Improve Vitamin D Levels:
Direct sunlight
Fatty fish, egg yolks, and fortified foods
Supplementation may be necessary
Liver Enzymes: ALT & AST

What Is It?
- ALT (Alanine Aminotransferase) and AST (Aspartate Aminotransferase) are enzymes found in the liver (and AST also in muscles, heart, and kidneys).
- When liver cells are stressed or damaged, these enzymes leak into the bloodstream → raising ALT or AST levels.
- They’re used as markers of liver health
Why It Matters?
- Chronically elevated ALT/AST can be an early sign of fatty liver disease, hepatitis, or toxic liver injury.
The AST: ALT ratio is sometimes used:
- ALT > AST → usually non-alcoholic fatty liver
- AST > ALT (especially >2:1) → may suggest alcohol-related damage
What Causes It To Be High?
- Non-Alcoholic Fatty Liver Disease (NAFLD) → strongly linked with obesity, insulin resistance, and metabolic syndrome
- Alcohol use
- Viral hepatitis (A, B, C)
- Medications or supplements (acetaminophen, statins, some antibiotics, herbal remedies)
- Muscle injury or strenuous exercise (AST especially)
- Autoimmune or genetic liver conditions
Tips To Improve Liver Enzymes:
Remove alcohol
Limit ultra-processed food and added sugar
Stay hydrated
Exercise regularly
Final Thought: Your Health Story Is Written in Your Numbers
Your health markers are more than just numbers on a lab report — they are early warning signs and progress trackers for your long-term health. From blood sugar and cholesterol to vitamin D and liver enzymes, each marker tells a piece of your health story. When you combine these insights with body composition testing, you gain a clear picture of whether you’re trending toward sickness, wellness, or fitness.
The good news? Most of these markers improve dramatically with simple lifestyle changes: eating balanced meals, moving your body regularly, getting quality sleep, and managing stress. Knowledge truly is power — and knowing your numbers gives you the power to prevent chronic disease, improve energy, and take control of your future.
At Healthy Steps Nutrition, our mission is to help you understand and optimize your health markers with practical, sustainable strategies. Whether it’s through annual blood work, nutrition coaching, or our Blood Sugar Balance Specialty Program with continuous glucose monitoring, you don’t have to figure this out alone.
Don’t wait until symptoms show up. Be proactive. Schedule your annual blood work, track your body composition, and take the small, consistent steps that will help you look, feel, and live better long-term.






